Achieving consistently strong hospice quality performance with predictive technology
Quality measures are an essential element of the hospice industry, encouraging accountability and providing transparency for potential patients and their families into how agencies perform. This allows them to differentiate higher from lower quality hospice settings. While these measures are important, hospice agencies face several challenges that can make consistently excellent performance difficult. Supported by the right tools, hospice teams are far more likely to succeed. So, let’s dive into the world of quality measures, why they can be difficult to meet, and how agencies can leverage predictive technology to get the help they need.
What kind of elements is CMS looking at?
To determine and report on hospice quality, CMS administers the Hospice Quality Reporting Program (HQRP), composed of four Quality Measures (QMs):
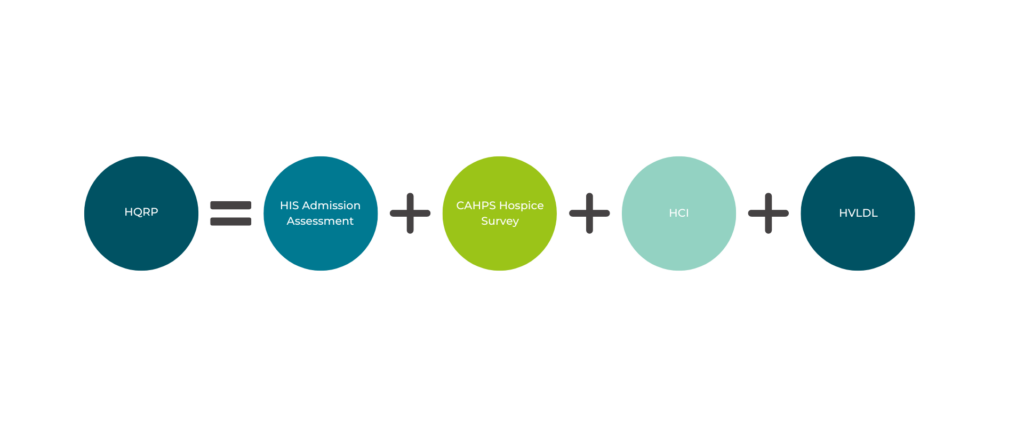
- HIS Comprehensive Assessment Measure at Admission: Measures the proportion of patients for whom hospice performed the seven care processes in the Hospice Item Set.
- CAHPS Hospice Survey: A set of eight CAHPS Hospice Survey measures including “Willing to Recommend this Hospice,” “Rating of This Hospice,” and various measures of patient and family support. These are key elements in decision making for families.
- Hospice Care Index (HCI) – A measure comprising ten indicators including “Visits Near Death,” “Burdensome Transitions”, and “Gaps in Skilled Nursing Visits.” These make it imperative for agencies to consistently understand their patients’ trajectory and how care is being provided relative to acuity. Scores range from 0-10.
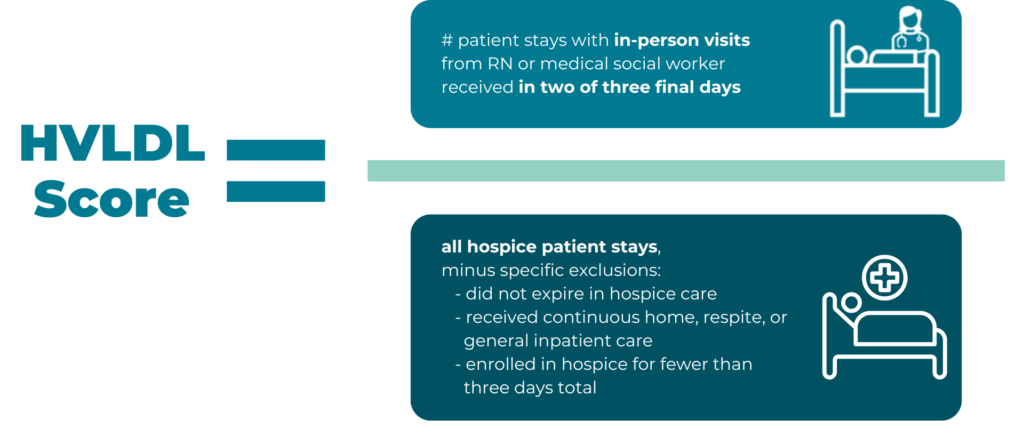
- Hospice Visits in the Last Days of Life (HVLDL), defined as the proportion of patients who have received in-person visits from an RN or medical social worker on at least two out of the final three days of life.
Quality care especially essential for patients closer to death
Patients and their families are in their moment of greatest need as a transition approaches. This is why HVLDL specifically is its own measure. To perform well on HVLDL, it’s essential for providers to recognize end-of-life indicators and changes in patient condition to accurately anticipate when a patient is likely to transition. Based on this understanding, agencies need to reliably concentrate visits and other resources on patients near transition. Consistent performance in this area also aligns with other elements of the HQRP like the “Visits Near Death” HCI indicator, as well as with the Service Intensity Add-On (SIA), a payment policy that incentivizes visits when patients are near death.
Beyond fulfilling their goal of providing high quality, compassionate patient care, agencies are rewarded financially for ensuring patients near death are appropriately cared for.
Consistent performance can be a challenge
While the importance of these measures – both to patients and providers – is clear, it can still be difficult for hospice agencies to consistently perform against HVLDL and other end-of-life focused metrics in the way they’d like to.
Part of the challenge is accurately understanding when a transition is coming. Patient records are complex, and a patient’s condition can change suddenly. Manually digging through lengthy records takes more time than most providers have. It also takes a good deal of thought to identify which elements of a patient’s complicated journey are most important in a given moment. In short, consistently and collectively evaluating diverse indicators to forecast transitions is difficult without help.
Another piece of the puzzle is that the staffing limitations inherent to the industry are exacerbated by visits being assigned where they may not be needed. Without continuous, patient-specific risk monitoring, agencies can find themselves assigning visits based on blanket rules and other factors divorced from transition likelihood. While it’s great that everyone is being seen, it’s not so great when there isn’t extra capacity to direct to those in the greatest need. Agencies must find a way to ensure that limited staff are free to make last days of life (LDL) visits as the need presents itself.
Hospice teams across the country have boosted their performance with Medalogix Muse
Right-sized, timely care in the last days of life is a key element of delivering a compassionate, less stressful experience for patients and families alike, which is the most important reason to get it right. It’s also essential for the continued operational success and quality scores of hospice agencies, which can more consistently perform against quality measures with the right tools.
With its Muse product, Medalogix has focused on helping hospice teams improve utilization and quality. Muse is a data science-driven technology that delivers dynamic clinical insights powered by machine learning in support of quality end-of-life care. Clear predictive insights empower clinicians with objective clinical data on a visit-by-visit basis to make informed decisions and improve quality of care.
Muse contains a wealth of features that help hospice teams optimize utilization by aligning with patient risk and appropriately concentrating visits on patients closer to transition. It’s also tailor made to give agencies direct visibility into elements that contribute to HCI and HVLDL. Beyond identifying patients in need of further action, Muse helps free up the capacity to follow through by presenting likely overutilization for lower-risk patients. While some visits saved by appropriate reductions in low-risk utilization can be reallocated to higher-risk patients, including end of life visits, others can be saved entirely.
Clients across the country have seen impressive results in these areas while using Muse, with performance on quality measures that far outpaces national averages. Today, Muse manages 20% of all Medicare Hospice patients. In 2023, clients leveraging Muse added an additional 450,282 visits during the last 7 days of life.

On average, Muse clients perform 45.3% better on HVLDL than the national benchmark, with improvements as high as 89% more patients meeting HVLDL visits. Clients like Amedisys, Avow, Bayada, Knute Nelson, and others have found great success with Muse, and we’re always working to improve the product further.
To learn more about what Muse can do for your agency and schedule a demo, visit our website!
Related Blogs
Navigating the Transition: How Medalogix Muse Supports Hospice Agencies in the Shift from HIS to HOPE
Authored by: Steven Shelton, MBA, MSN, RN, CHPN; Senior Director, Clinic...

Forcura and Medalogix Join to Create Transformative Post-Acute Care Technology Platform
Berkshire Partners Will Serve as Lead Investor in the New Platform, with...

HHVBP: A Winning Strategy for Home Health Providers
The start of 2025 has ushered in a wave of new realities for Home Health...


