Unlocking Efficiency and Precision in Home Health Documentation
Home health teams operate in diverse and uncontrolled settings, ranging from private residences to assisted living facilities, where distractions and interruptions are commonplace. Combine this with lengthy and complex patient records, staffing challenges, and the pressure to document quickly, and it all adds up to the perfect storm for documentation inaccuracies. These inaccuracies ultimately impact time, costs and reimbursements, and patient outcomes.
Documentation burdens consistently contribute to lower work satisfaction and burnout for healthcare professionals, particularly without the right tools. Formal clinical documentation improvement (CDI) teams and processes have long been part of hospital workflows, which has given both processes and technologies time to mature in the hospital space. Home health, however, has lagged behind, despite the persistence of uniquely difficult documentation challenges. Some traditional CDI responsibilities are distributed across agencies, but consistent, formalized processes aided by technology are uncommon.
In their 2024 Home-Based Care Outlook Survey and Report, Homecare Homebase and Home Health Care News asked where companies could achieve the greatest efficiencies in 2024. Home health professionals identified staffing utilization (27%), process optimization and automation (25%), and referrals (19%) as their top three priorities. Among those who anticipated investing in technology, the top goals for that investment were to:
- improve patient outcomes and monitoring,
- reduce operating costs, and
- correct ineffective documentation processes.
In short, the needs and goals of agencies across the industry align well with the positive impacts and outcomes yielded by CDI technology.
With that in mind, let’s dive into the world of documentation integrity, the challenges to consistently producing high-quality documentation, and some recommendations for how home health organizations can leverage predictive analytics for better patient, operational, and financial outcomes.
Strong documentation practices are key to high-quality care, accurate coding, and reimbursement
CDI is a systematic approach aimed at producing more accurate, complete, and specific clinical documentation that fully reflects the severity of the patient’s condition and the intensity of care provided. CDI processes typically involve comprehensive documentation reviews by trained professionals, such as CDI specialists, who work with clinicians to ensure that diagnoses, treatments, and procedures are accurately recorded and to promote adherence to coding guidelines and regulatory requirements. This has both clinical and revenue cycle impacts, and improves the patient experience.
The importance of complete and accurate clinical documentation stems from its serving as (i) a reference point for decisions on care provision and (ii) a foundation for coding, OASIS, and other elements that determine reimbursement levels for home health agencies. CMS’s implementation of the Patient-Driven Groupings Model (PDGM) case-mix and payment classification system made accurate documentation more important than ever.
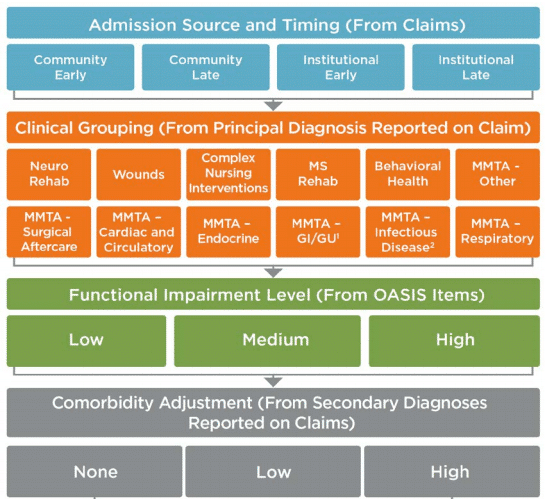
PDGM is intended to more accurately align reimbursements to documented patient acuity and care needs. There are 432 possible case-mix adjusted payment groups, with each corresponding to a different level of payment to the provider because statistically, patients with higher acuity require more (and more expensive) care. The inherent complexity in the PDGM model means mistakes are inevitable without help. Resulting documentation deficiencies have consequences, including imperfect care as well as net undercoding and underpayment issues:
- Patient experience and outcomes: Where documentation fails to fully capture the patient’s condition, care planning, continuity, and quality are impacted. Missing detail can lead to suboptimal treatment plans, delays, unnecessary hospital readmissions, or adverse health outcomes. This hurts both patients and their families alike.
- Inaccurate coding and reimbursement: Because coders reference clinical documentation as they work, deficient documentation leads to deficient coding. While overcoding can occur, organizations almost always have a net undercoding issue. This leads to lower reimbursements that don’t reflect the work they perform or the case mix of their patient census.
- Quality measures (e.g. CMS Star ratings): If the severity of a patient’s condition is not accurately documented, and they experience health outcomes that should not have occurred given documented acuity, providers appear to perform poorly relative to patient condition. Conversely, if a patient experiences negative outcomes that align with higher acuity, this is more in line with expectations.
- Agency administration: Inaccurate OASIS data and other documentation issues can skew statistical analyses and reporting used for quality improvement initiatives. Agencies rely on this data to identify trends, assess their performance, and implement improvements.
Despite its importance, clinical documentation has presented a persistent challenge in home health
Given all the negative outcomes of inaccurate or incomplete clinical documentation, why haven’t agencies fixed the problem? Ultimately, it’s a challenging issue to solve without the right tools. As it is throughout the healthcare industry, staffing is a challenge in CDI. Even well-staffed CDI initiatives have weaknesses, though, if they depend on manual reviews. Let’s look at referral and admission processing as just one example.
Assuming an average referral packet of 50 pages, reading benchmarks suggest that initial processing of the average referral should take about 75 minutes per patient. Best case, there are immense inefficiencies with time spent per record, assuming absolutely nothing is missed. We know, however, that diagnoses, comorbidities, and other elements that impact PDGM are regularly missed. What’s more, admitting clinicians often don’t have the time needed to dig through lengthy records in preparation for admissions visits. Documentation and the patient experience are already starting off on the wrong foot.
In short, manual processing consumes valuable administrative time and increases the risk of errors and delays in initiating patient care. The lack of standardized referral processes and communication channels between referring physicians and home health agencies further exacerbates the challenge. Clinicians often encounter incomplete or inconsistent referral information, requiring time-consuming follow-up and clarification. These inefficiencies can hinder timely care and strain relationships with referring providers.
Leveraging technology to analyze and surface key insights from lengthy referral documentation frees up clinicians to focus on areas where their unique clinical expertise is most needed. Streamlining referral processing through automated systems and standardized protocols is essential to overcoming these challenges and optimizing the delivery of home health care.
Clinical documentation improvement efforts are amplified by the right technology.
Home health organizations serious about addressing the challenges of complete and accurate documentation can benefit greatly from the right technology. In their report “Investing in the new era of value-based care,” McKinsey recommended that “successful value-based care providers will increasingly need to look into more innovative levers to maintain value.” Among the value sources cited are:
- Improvements to risk-coding accuracy to capture health status
- Prediction of health risk status
- Improved performance on Star ratings and other quality measures
- Reduction in potentially avoidable hospital readmissions
Home health agencies can realize these and other benefits with advanced technologies like artificial intelligence, natural language processing, and predictive analytics. These tools streamline documentation workflows, empowering clinicians to capture comprehensive patient information efficiently. By optimizing clinical documentation, CDI technology not only supports accurate reimbursement and quality reporting but also fosters improved clinical decision-making and patient care outcomes. In this way, it serves as a more effective bridge between clinicians, caregivers, and administrators.
Medalogix’s new Referrals & Admissions module, part of the comprehensive Pulse home health platform, applies machine learning AI to autonomously perform complex, lengthy reviews in a small fraction of the time it would take a human to manually review. It condenses referral records into a single-page, cross-linked clinical summary and surfaces key insights from the patient record relevant to each element of PDGM. This enables a level of thorough review and consistent accuracy that was nearly impossible before, while reducing time spent on administrative tasks and allowing clinicians to focus more on direct patient interaction. Ultimately, agencies can see improved admissions visits, referral decisions, and time to admission, with evidence-based coding and Focus of Care for reimbursements that better reflect your patients’ acuity and the care you provide them.
A few final thoughts
In the realm of home healthcare, documentation is pivotal yet challenging. Home health clinicians juggle diverse environments, limited resources, and dynamic patient conditions, all while striving to maintain accurate records.
The great news for agencies, clinicians, and patients alike is that better tools than ever are available to ensure timely documentation processing and alignment between patient condition, coding, and reimbursement. Pulse Referrals & Admissions was purpose built to solve these issues, and can lead to rich benefits:
- CDI empowers clinicians to make informed decisions, personalize treatment plans, and anticipate health complications proactively.
- Standardized documentation facilitates seamless care transitions and enhances coordination across the continuum, promoting patient safety and satisfaction.
- By accurately capturing patient acuity, CDI ensures precise coding of diagnoses and procedures, maximizing reimbursement potential and maintaining compliance.
- Standardized documentation practices enhance operational efficiency, reducing overhead costs associated with manual processes
- Enhanced communication between clinicians and coding staff reduces coding errors, fostering transparency and accountability in healthcare delivery.
In the face of persistent challenges, Pulse Referrals & Admissions offers a transformative solution, unlocking efficiencies, driving financial sustainability, and enhancing patient care outcomes. By embracing tools like these, home health organizations can navigate the complexities of documentation, optimize resource utilization, and ultimately, deliver exceptional care to those they serve.
Learn more about Referrals & Admissions and our full home health platform software solution.
Related Blogs
Navigating the Transition: How Medalogix Muse Supports Hospice Agencies in the Shift from HIS to HOPE
Authored by: Steven Shelton, MBA, MSN, RN, CHPN; Senior Director, Clinic...

Forcura and Medalogix Join to Create Transformative Post-Acute Care Technology Platform
Berkshire Partners Will Serve as Lead Investor in the New Platform, with...

HHVBP: A Winning Strategy for Home Health Providers
The start of 2025 has ushered in a wave of new realities for Home Health...


