Solving the Home Health Maze: Referral & Intake
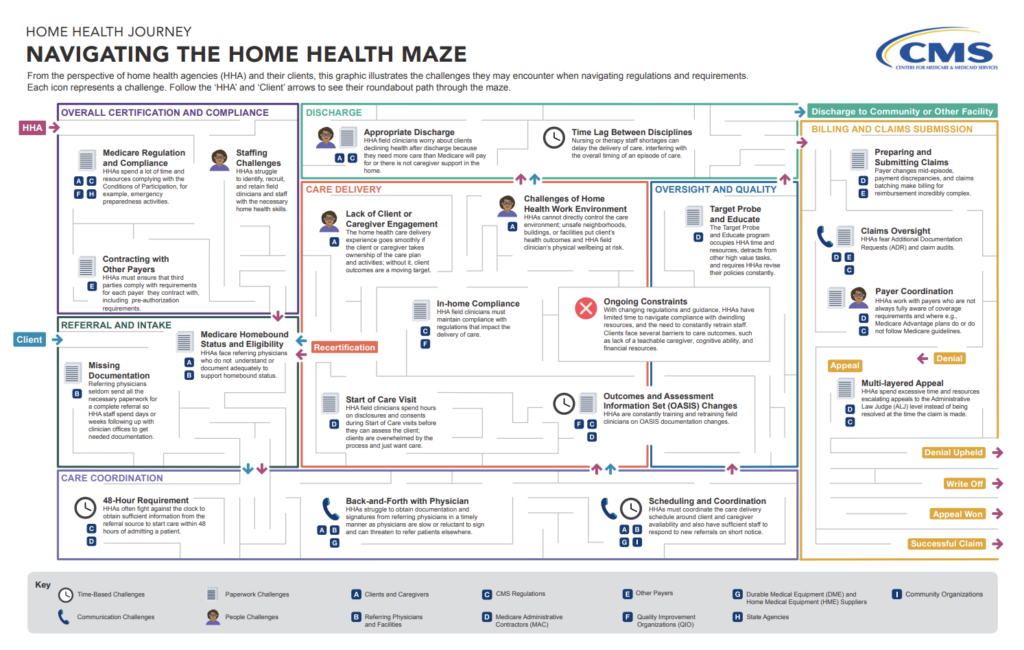
The CMS Office of Burden Reduction & Health Informatics (OBRHI) collaborates with stakeholders across the healthcare spectrum to identify and address inefficiencies, improving access to quality, affordable care. Their recent publication, “Navigating the Home Health Maze,” sheds light on the multifaceted challenges and regulatory complexities faced by Home Health providers. While this resource effectively outlines high-level obstacles across patient episodes, it falls short of providing the nuanced details behind today’s operational challenges. This article aims to explore the challenges and opportunities related to processing referrals and intake, and the downstream impacts on care, claims, and outcomes.
Referrals
The demand for Home Health care continues to rise, but access remains a difficult challenge. Recent reports indicate a concerning 41% increase in rejection rates among Home Health agencies compared to the previous year. This increase builds upon an already troubling record high 76% rejection rate across the industry. This surge is compounded by the fact it takes 70 minutes to fully review an average referral packet to get to an informed admit or decline decision by intake coordinators. A Medalogix analysis of admitted patients reveals that, on average, each patient admission packet comes with two associated documents totaling approximately 35 pages. Extreme cases involve patients with up to 25 documents and nearly 300 pages of clinical information. Once a referral has been accepted, providers have 48 hours to complete the initial assessment visit.
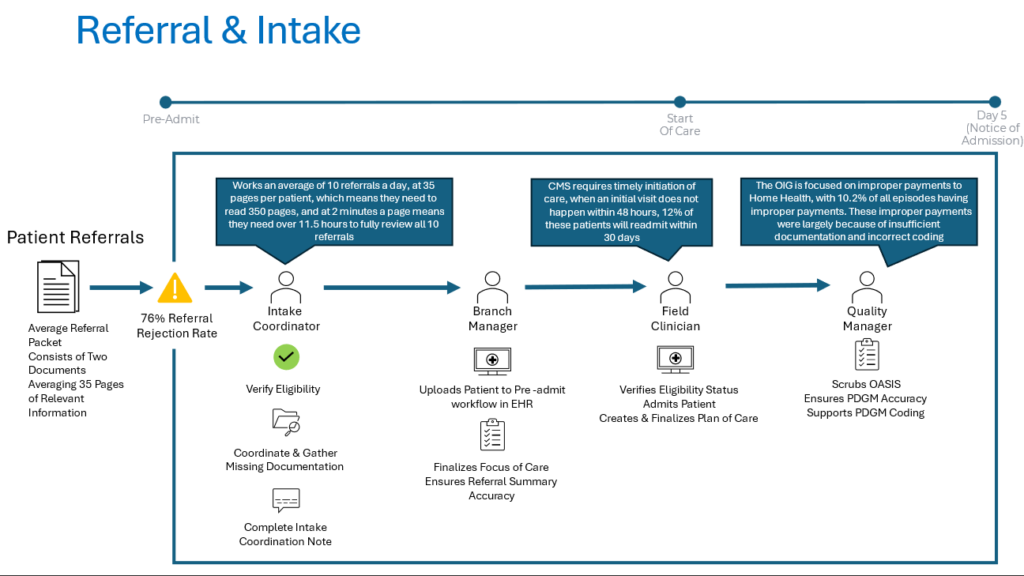
In spite of the volume of patient information, intake coordinators are tasked with swiftly assembling a more complete view of the patient and services required, soliciting missing data, and facilitating the admission process. Forward-thinking providers are turning to technology to streamline referral management, automate manual workflows and create efficient communication between teams. Savvy providers are leveraging Forcura’s IQ technology, which instantly identifies and populates critical data points like patient demographics, referral source and payer from all referrals in a single dashboard view. In a click, providers can prioritize those referrals for patients who reside in their service area, are referred by preferred sources, and fit their payer mix. Forcura’s referral summary, powered by generative AI technology, instantly summarizes patient referral packets and serves up essential clinical information including primary diagnosis and services ordered, patient status and certifying physician. The result: providers can make faster, more informed admit or decline referral decisions.
“It’s validating to hear our clients call Forcura IQ “life-changing,” because that’s 100% the impact we hoped it would have,” says Craig Mandeville, founder and CEO of Forcura. “When providers are expected to care for higher acuity patients, deliver care with fewer staff, and operate under threat of more CMS cuts and claw backs, it’s our duty to equip them with tools that decrease some of these administrative burdens and enhance their productivity.”
Leveraging intelligent tools to serve up data and summarize referral packets is revolutionizing the process, expediting decision-making, and facilitating prompt patient admissions.
Intake
Once a patient has been accepted by the agency, the provider has only 48 hours to conduct the admitting visit. On average, over 30% of episodes have delayed starts of care. A study found that 12% of patients who experienced a delayed start of care readmitted within 30 days. From the initial assessment visit, providers have a regulatory requirement to provide notice of admission within 5 days. Compounding this requirement is the coordination of activities from in-field clinicians to branch managers to quality managers, not to mention, cross-disciplinary coordination for care planning and quality documentation, and OASIS scrubbing and coding. For some, this includes leveraging 3rd party coding and scrubbing vendors. During this phase, staff members must accurately review all patient data to establish a focus-of-care, finalize plan-of-care, while ensuring accurate coding is being presented to CMS.
A review of recent studies has found that patients transitioning from hospital to home were affected by at least one medical error and 20% were affected by one or more adverse events. These events can be the result of missed or conflicting information buried deep in the patient referral packet, clinical documents or EHR. These adverse events or rehospitalizations can have a negative impact on agency reputation, CMS 5-Star, negative Home Health Value-Based Purchasing (HHVBP) scores, and impact relationships with referring partners.
The process is further complicated by recent announcements from the U.S. Department of Health and Human Services Office of Inspector General (HHS-OIG) regarding improper payments to Home Health. In 2021, the improper payment error rate for home health stood at 10.2%. Likewise, a recent Medicare report identified insufficient documentation (68%) and incorrect coding (22%) as primary contributors to improper payments for Part B.
To help providers overcome the operational and regulatory challenges admitting a new patient, Megalogix launched Pulse Referrals and Admissions. Using the latest large language model (LLM) AI to provide review, cross referencing, and insight capabilities that supercharge intake and admission teams. Summarize complex referrals in a fraction of the time needed for manual review, then leverage intelligent insights to compare and align referral documents, OASIS assessments, and clinical notes with patient needs.
Medalogix’s analysis of completed patient episodes, utilizing Pulse Referrals and Admissions to evaluate clinical documents available during the intake process, underscores significant disparities in patient coding and focus of care. Coding analysis indicates that 47% of patients had documented clinical needs that were overlooked and 10% were likely subject to compliance issues, with only 43% requiring no correction or further action.
“Medalogix has been leveraging Home Health assessment information to generate plan of care recommendations for more than a decade.” Said Elliott Wood, President and CEO of Medalogix. “As such, we recognize how critical it is to ensure the documentation is timely and accurate. To help providers understand areas of opportunity, we are now offering to review a limited number of patients in Pulse Referrals and Admissions at no charge. Better documentation for the patient ensures better awareness for the cross-functional clinical teams and drives better care planning, delivery and ultimately, improved outcomes. Incorrect documentation not only impacts the customer in terms of improper reimbursement, but also potentially impacts the patient and their ability to have a successful episode of care in their home.”
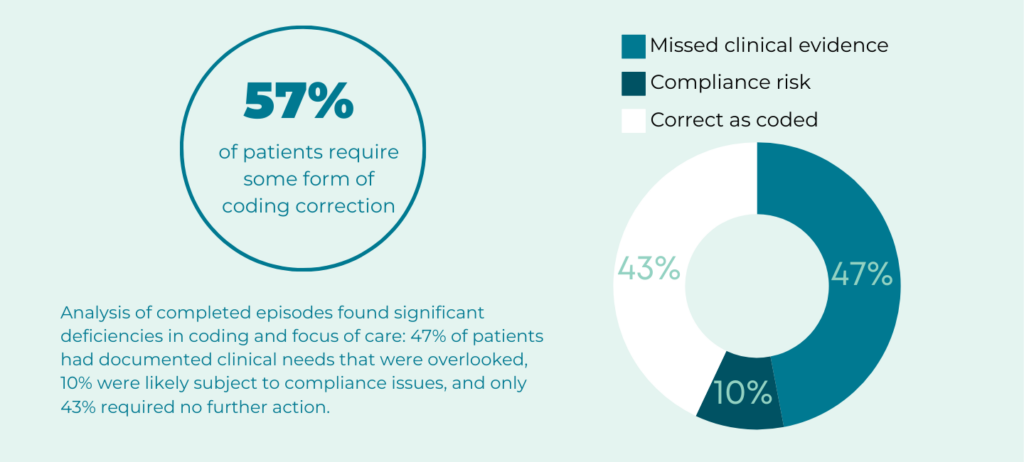
It’s critical not only that a patient’s plan of care and coding accurately reflect their needs, but also that agencies can provide supporting evidence from source documentation to not only support care coordination but also provide reference materials should CMS-OIG request more information. Medalogix Pulse Referrals and Admissions looks at all relevant patient information (referral documents, Oasis Assessment, and clinician notes) to create a simplified two-page PDGM summary. Using generative AI, providers can quickly review pertinent patient information, capture source reference information, and leverage AI to provide supporting insights or identify conflicts that could create errors, impacting patient care. Our analysis indicates that AI is identifying errors in documented primary diagnosis, OASIS and co-morbidities in 57% of all patients analyzed.
Solving the Referral and Intake portion of the Home Health Maze can be simplified by partnering with organizations like Forcura and Medalogix. Creating efficiencies from pre-admit to notice of admission can have significant impacts to patient care, operational improvements, and enhanced financial outcomes. Discover more by visiting Forcura or Medalogix.
If your organization is struggling to navigate the Home Health Maze, especially referrals and intake, Medalogix is offering a unique risk-free opportunity to evaluate your patients using Pulse Referrals and Admissions to provide a comprehensive analysis of opportunities to improve patient outcomes. Request your free analysis by clicking here.
Related Blogs
Navigating the Transition: How Medalogix Muse Supports Hospice Agencies in the Shift from HIS to HOPE
Authored by: Steven Shelton, MBA, MSN, RN, CHPN; Senior Director, Clinic...

Forcura and Medalogix Join to Create Transformative Post-Acute Care Technology Platform
Berkshire Partners Will Serve as Lead Investor in the New Platform, with...

HHVBP: A Winning Strategy for Home Health Providers
The start of 2025 has ushered in a wave of new realities for Home Health...


