Proactively addressing hospice revocation risk
While hospice care is the best end-of-life care option for most patients and families, sometimes they decide to revoke their hospice enrollment. This can have unintended impacts on the kind of care the patient receives while also creating challenges for hospice agencies. Fortunately, there are steps providers can take to better anticipate, address, and prevent hospice revocations to benefit patients and their families. By applying predictive analytics, agencies can help patients receive the kind of education, care, and resources they need to make the best care decisions at a critical time in their care journey.
Hospice revocations impact both patients and agencies
As patients approach the end of their life, hospice is generally the best setting for them and their families with its balance of physical, spiritual, and emotional support. It also preserves the ability to remain in a familiar setting at home. Taken together, this affords patients a kind of care better suited to the end-of-life period than standard home health or (especially) acute care. Focused on comfort in a time of great physical and emotional need, hospice care is also inherently less interventionist. As such, decisions to enroll in hospice care should be made with a full understanding of what it is and is not.
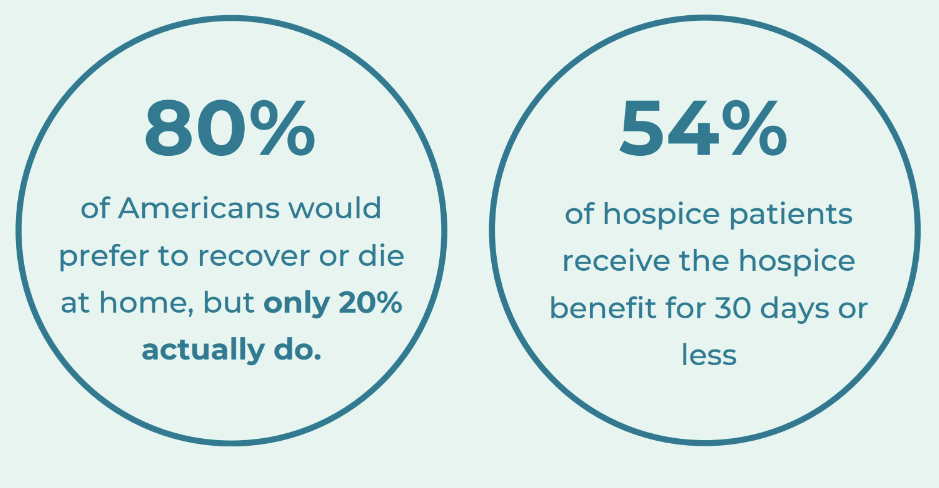
In hospice care today, nearly 1 in 5 patients will discharge prior to death, which is known as a live discharge. While some live discharges occur for reasons that have no connection to quality of care (e.g., ineligibility or relocation), revocations are a subset of live discharges that occur when a patient or their representative intentionally and specifically revokes enrollment in hospice care. When patients revoke, they are often not aware of what they are turning down, and may find themselves in a more stressful, less supportive environment.
While patients who revoke will likely miss out on the kind of care best suited to their condition as they near end of life, revocations also impact hospice providers. This impact is multifaceted and includes potentially negative movement on quality metrics, decreased revenue, and increased audit risk, which brings added costs and complications:
- Revenue and operational impacts: When patients revoke their hospice enrollment, this can result in a loss of revenue for the hospice agency as patient days on the hospice census are reduced. In addition, there are operational consequences with the administrative and clinical burden of taking on new patients following revocations.
- Impact on quality metrics: Part of the CMS Hospice Quality Reporting Program (HQRP), the Hospice Care Index (HCI) includes four indicators that are most clearly impacted by revocations:
- Early Live Discharges, calculated as the percentage of live discharges within the first seven days after hospice admission.
- Late Live Discharges, defined as the percentage of live discharges on or after 180 days after hospice admission.
- Burdensome Transitions (Type 1): the percentage of live discharges from hospice with a hospitalization within two days that is followed by hospice readmission within two days of hospital discharge.
- Burdensome Transitions (Type 2): the percentage of live discharges from hospice with a hospitalization within two days, where the patient also dies during the inpatient hospital stay.
Revocations open the door to poor scores on these indicators, where if an agency is performing below the 90th percentile, they don’t receive a point. Poor performance on quality metrics more broadly can do reputational damage that can impact an agency’s competitiveness.
- Audit risk: As Hospice News points out, “The U.S. Centers for Medicare & Medicaid Services (CMS) and the U.S. Department of Health & Human Services Office of the Inspector General (OIG) have been closely eyeing live discharge rates. These have become a frequent trigger for audits, which can be expensive and time consuming for a hospice.” While some live discharges aren’t preventable, revocations can be, and improving revocation rates can help alleviate audit risk.
Why do patients revoke?
A peer-reviewed study in the Journal of Palliative Medicine surveyed a range of hospice providers and found eight core themes in the reasons behind revocation: (1) not fully understanding hospice, (2) lack of clarity about disease prognosis, (3) desire to continue receiving care from nonhospice physicians and hospital, (4) caregiver burden, (5) distressing/difficult-to-manage signs and symptoms, (6) caregivers’ reluctance to administer morphine, (7) 911’s faster response time compared to hospice, and (8) families’ difficulty accepting patients’ mortality. Among these, distressing symptoms, a lack of understanding about hospice, and difficulty accepting a patient’s mortality were mentioned the most frequently.
The prevalence of these themes is understandable, and despite the negative impacts of revocations, hospice agencies can struggle to prevent them. Looking at revocation as the result of distressing symptoms, for instance, it can be challenging toconsistently and accurately understand a patient’s risk profile and trajectory. Patient records are lengthy and complex, and a change in patient condition, and resultingly disposition, can come suddenly. In addition, ubiquitous staffing challenges in healthcare make timely response even more difficult. When hospice teams aren’t appropriately responsive, a patient may respond by opting out. The same thing can happen when a patient’s family isn’t getting the support they need medically or emotionally from hospice care. Thankfully, these causes of revocation can often be anticipated and addressed.
Medalogix Muse helps forecast and prevent hospice revocations
Given the volume of patient data and the number of things care providers must attend to at any given time, giving sufficient attention to revocation risk is nearly impossible without assistance. Continual manual analysis of this data takes far too long for the kind of timely action needed to address deficiencies that may impact a patient’s decision. That’s where Medalogix Muse comes in, helping inform the development of treatment plans tailored to individual acuity and priorities, enhancing quality of life and managing symptoms effectively. This creates a hospice environment where the patient and their family feel supported and comfortable, preventing revocations.
Leveraging breakthrough data science models trained on data from hospice agencies across the country, Muse identifies patients who are 5 times more likely to revoke within 30 days than other patients on the census. These patients are easily reviewable with an at-a-glance widget on Muse’s homepage. Predictions are refreshed with every skilled nursing visit and are rooted in exhaustive analysis of patient data — assessments, diagnosis, narrative notes, medications, vitals, and more. Once a patient is identified as a revocation risk, care teams can identify where to insert a tuck in call or phone visit, where patients could benefit from additional education, where there is an opportunity to leverage volunteer services, and more.
Intelligent prompts direct attention to where it is most needed to address potential revocations and ensure a level of patient care that leaves them feeling fully supported. Analysis of Muse users already demonstrates lower revocation rates, with a nearly 20% decrease in the number of live discharges that are revocations. Medalogix is uniquely positioned to deliver this benefit, with recommendations based on data science models trained on over 1 billion attributes, 749 million words, and 14.5 million unstructured patient data points.
Beyond the patient, these adjustments help agencies align with quality best practices, for example with relation to the HCI metrics mentioned above. With HCI being scored from 0-10, the loss of even a couple points can have a major impact on the reputation and competitiveness of an agency in the marketplace. Muse as a whole goes beyond revocation risk reduction, featuring elements that address every HCI indicator:
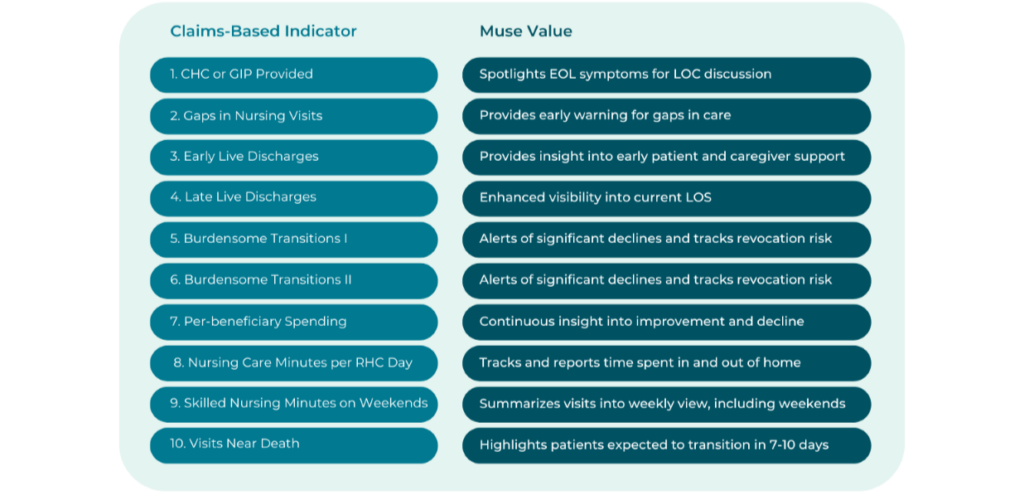
In short, the predictive analytical capabilities Muse help agencies directly address care planning and provision challenges to provide comfort and right-sized care to patients, reduce revocation risk, and strengthen quality performance.
Final thoughts
Providing hospice care that meets patient and family needs in a physically and emotionally difficult time is a challenge, but it’s a challenge providers can better meet with the right tools. By proactively identifying patients at risk of revocation and working to address their needs for education, additional visits, and other resources, agencies can help patients continue to receive the best possible care in the right setting.
Medalogix products are built with a clear focus on helping patients receive the ideal type and level of care for their condition at any given time. Because hospice is generally the preferred option as a patient near the end of their life, revocations are an outcome that agencies should proactively work to prevent. Muse now includes tailor-made functionality to address this challenge. Clients across the country have seen impressive results while using Muse, with performance on quality measures that far outpaces national averages. Today, Muse manages 20% of all Medicare Hospice patients. In 2023, clients leveraging Muse added an additional 450,282 visits during the last 7 days of life. To learn more, visit our Muse page and schedule a demo.
Related Blogs
Navigating the Transition: How Medalogix Muse Supports Hospice Agencies in the Shift from HIS to HOPE
Authored by: Steven Shelton, MBA, MSN, RN, CHPN; Senior Director, Clinic...

Forcura and Medalogix Join to Create Transformative Post-Acute Care Technology Platform
Berkshire Partners Will Serve as Lead Investor in the New Platform, with...

HHVBP: A Winning Strategy for Home Health Providers
The start of 2025 has ushered in a wave of new realities for Home Health...


