How hospice providers can flourish in an increasingly value-based care environment
Value-based care is the future of hospice
Hospice care is critical to the broader healthcare ecosystem, affording compassionate care to patients and families in their time of greatest physical and emotional need. Over the past several years, the Centers for Medicare and Medicaid Services (CMS) have made several moves that have furthered the importance of value-based care in the hospice space. This multi-year trend signals a deeper future structuring around value-based care for which agencies should prepare now.
Value-based care emphasizes quality of care and efficient use of resources, but most importantly the principle of patient-centeredness. This model encourages providers to holistically meet patient needs and drive positive outcomes relative to condition. It also ensures that treatment plans are tailored to individual acuity and priorities, enhancing quality of life and managing symptoms effectively. At the organizational level, value-based care drives optimization of staffing levels, utilization of evidence-based practices, and effective communication, all key to agency sustainability.
Existing quality reporting infrastructure makes the provision of quality patient care, rooted in right-sized utilization and strong outcomes, imperative to the success of the modern hospice agency. These metrics encompass various aspects of care delivery and help determine the relative performance of hospice options under consideration. Because of the connection between quality performance and care delivery costs, these metrics can also impact negotiations with payers and network access.
As Hospice News points out, “Not only is delivering quality services the right thing to do for patients, it will be a key to success when working within a value-based reimbursement environment, whether it be for hospice care or other services like palliative care or PACE. Demonstrating both quality outcomes and reduced health care costs will be an important part of hospices’ competitive edge – regardless of a provider’s size, geographic reach or tax status.”
Hospice agencies can struggle to consistently perform against quality metrics
Despite the clear importance of the hospice space’s ongoing pivot towards value-based care, consistently strong performance on quality metrics can be a challenge for agencies. Part of the struggle comes from the challenge of accurately understanding a patient’s risk profile and trajectory. Patient records are lengthy and complex, and a change in patient condition can come suddenly. Hospitalizations, revocations, and other issues can arise when teams aren’t appropriately responsive. Consistently and comprehensively evaluating diverse risk indicators is difficult for even the best teams to accomplish manually.
This may seem like the kind of problem that additional staffing can solve. In the 2024 Hospice News Outlook Survey and Report, however, staffing remains the top challenge hospice agencies report facing. Twice as many respondents cited staffing (36%) as a concern versus the next-highest challenge reported (17%). Even if an agency has an ideal staffing level, understanding changes in patient needs and acuity can be difficult. This makes utilization misalignment a consistent problem. Agencies often assign excess visits to low-risk patients, leaving gaps in care for higher-risk patients nearing the end of their life, which in turn impacts quality metrics like HVLDL.
These challenges, inherent to working in hospice, introduce a gap between the ideal level and type of care a patient should receive based on their condition and the reality of day-to-day operations. Agencies can overcome this gap with targeted application of the right technologies. This augments staff capacity and introduces improved practices to an agency.
Predictive analytics empower hospice teams to provide quality care
Predictive analytics fits neatly into the gap between ideal quality patient outcomes and the reality of how agencies generally perform. Solutions like Medalogix Muse are revolutionizing hospice care by providing deeper insights into patient needs and prognosis. Leveraging data from throughout complex patient records, Muse forecasts patient outcomes, identifies risk factors, and helps personalize care plans. Built on an immense data set (14.5 million unstructured data points, 749 million words, 1.1 billion attributes), Muse analyzes trends and patterns in patient data to present visit-by-visit recommendations to hospice teams. This allows them to proactively address symptoms, anticipate care needs, and optimize utilization to improve patient outcomes and operations alike.
Agencies that align themselves with CMS quality metrics through leveraging predictive analytics solutions like Muse can ensure that every patient receives compassionate, high-quality care tailored to their needs. As the importance of value-based care in hospice deepens, the integration of innovative approaches is essential to patient outcomes and agency performance.
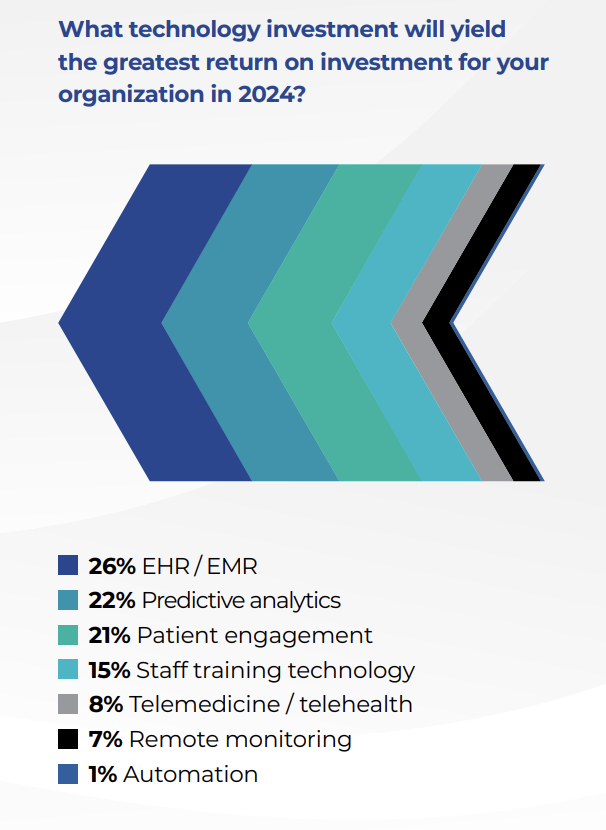
The 2024 Hospice News Outlook Survey and Report also identified key areas of technology investment for hospice. Muse, at its core a predictive analytics solution, also addresses patient engagement by identifying where agencies can better allocate resources to meet patient needs.
Muse helps agencies target performance on HCI indicators
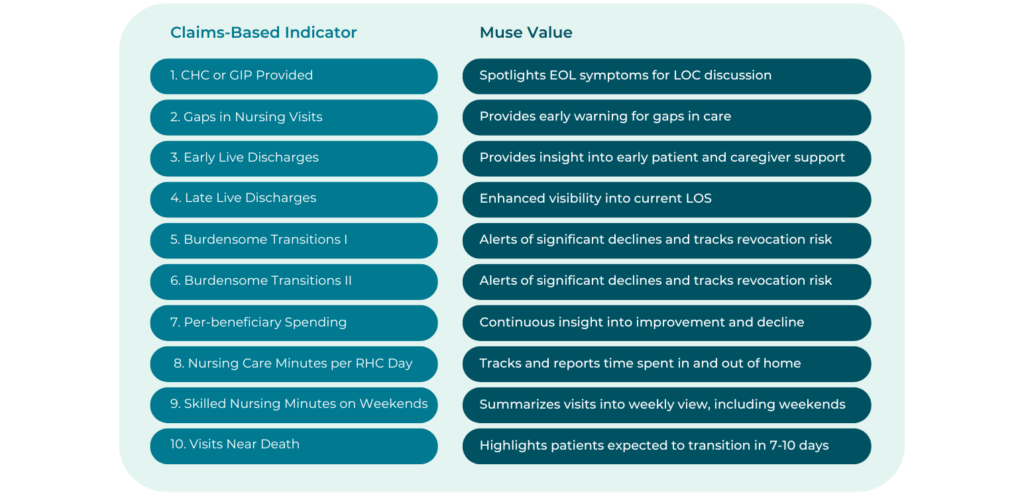
Central to Muse is a multifaceted focus on helping agencies perform well against the quality metrics used by regulatory bodies and prospective patients to judge hospice agencies. In short, we go beyond just talking about the importance of quality by directly addressing individual quality metrics:
Various features within Muse were purpose-built to address the 10 HCI indicators. Most recently, Muse has seen the addition of revocation risk reduction functionality, which drives further attention to four of these indicators:
- Early Live Discharges, calculated as the percentage of live discharges within the first 7 days after hospice admission. If agencies struggle in this area, it can suggest problems with care or program quality, a failure to meet patient or family needs, or frequent admission of non-eligible patients.
- Late Live Discharges, defined as the percentage of live discharges on or after 180 days after hospice admission. Poor performance could indicate an agency is seeking out patients likely to have long stays but don’t meet eligibility criteria.
- Burdensome Transitions (Type 1): % of live discharges from hospice with a hospitalization within two days that is followed by hospice readmission within two days of hospital discharge. Agencies struggling here may have deficiencies in proactive care planning around hospitalization prevention and discharge practices that don’t identify patients with stabilized conditions.
- Burdensome Transitions (Type 2): % of live discharges from hospice with a hospitalization within two days, where the patient also died during the inpatient hospital stay. Again, this could suggest discharge processes that don’t look at patient stability prior to live discharge.
Using Muse, agencies can identify where resources used for tuck invisits, calls, education, and volunteer services could have the most impact in preventing a revocation. Strong performance on each of these metrics is key, since CMS only awards points if an agency is at or above the 90th percentile. With HCI being scored from 0-10, the loss of even a couple points impacts the reputation and competitiveness of an agency in the marketplace. Beyond just revocation risk reduction, Muse contains elements that address every HCI indicator:
Muse has further quality impacts across HQRP metrics
Hospice Visits in the Last Days of Life (HVLDL): Patients and their families are in their moment of greatest need as a transition approaches. It’s especially important for providers to recognize end-of-life indicators and changes in patient condition to accurately anticipate when a patient is likely to transition. This is where HVLDL comes in, as well as other elements like the “Visits Near Death” HCI indicator. Muse helps free up the capacity for improved HVLDL performance by presenting likely overutilization for lower-risk patients. Some visits saved by appropriate reductions in low-risk utilization can be reallocated to higher-risk patients, including end of life visits. Others can be saved entirely. With better end-of-life care comes improved Service Intensity Add-On (SIA) payments, so patients and agencies both benefit from aligning visits to patient condition.
CAHPS Hospice Survey: This survey is a set of eight CAHPS Hospice Survey measures, including “Willing to Recommend this Hospice” and “Rating of This Hospice.” It touches various measures of patient and family support and is a key element in decision making for families. By ensuring care alignment with patient condition and recommending additional visits and other resources as needed, Muse helps agencies provide patients and their families with the kind of compassionate experience that leads to strong CAHPS survey performance. This ultimately leads to a stronger reputation in the marketplace and census growth.
Final thoughts
Like countless providers across the country, Medalogix is focused on the patient. We want them to receive compassionate, quality care that meets their needs and makes a difficult time easier. We also recognize the reality of CMS structuring around value-based care, and the demands this places upon agencies. With all of this in mind, Muse was built to help agencies deliver the best care possible. It’s also tailored to driving strong performance against quality metrics. Clients across the country have seen impressive results using Muse, with quality performance that far outpaces national averages. Today, Muse manages 20% of all Medicare Hospice patients. In 2023, clients leveraging Muse added an additional 450,282 visits during the last 7 days of life. To learn more, visit our Muse page and schedule a demo.
Related Blogs
Navigating the Transition: How Medalogix Muse Supports Hospice Agencies in the Shift from HIS to HOPE
Authored by: Steven Shelton, MBA, MSN, RN, CHPN; Senior Director, Clinic...

Forcura and Medalogix Join to Create Transformative Post-Acute Care Technology Platform
Berkshire Partners Will Serve as Lead Investor in the New Platform, with...

HHVBP: A Winning Strategy for Home Health Providers
The start of 2025 has ushered in a wave of new realities for Home Health...


