Expertise

Announces Release of Pulse Referrals & Admissions Modules Backed by Generative AI
Pulse modernizes admissions workflows with proprietary documentation imp...
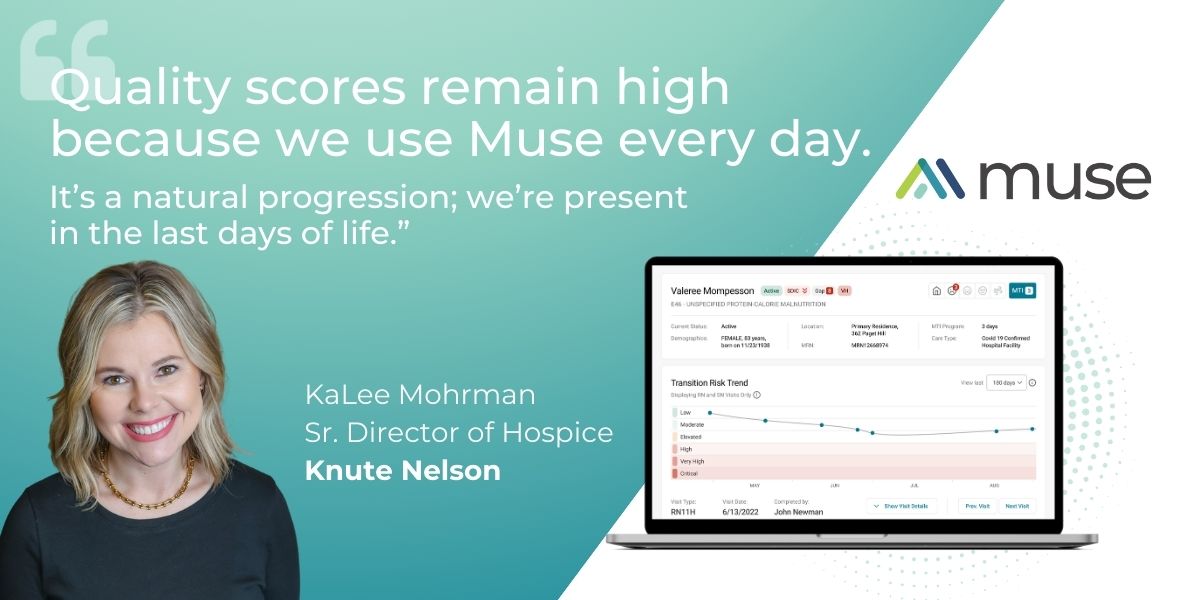
Improving Hospice Care with Data-Driven Insights: A Conversation with Knute Nelson Hospice
Providing compassionate and high-quality support to patients and their f...

The FY 2024 Hospice Payment Rate Update Proposed Rule: Why Quality Matters Even More
By: Cyndi Rizzitello, MSN, RN, BC On March 31, 2023, the Centers ...

Unlocking Efficiency and Precision in Home Health Documentation
Home health teams operate in diverse and uncontrolled settings, ranging ...

High-quality, accessible data essential to strong home health practices and outcomes
When it comes to providing quality home health care, agencies are only a...
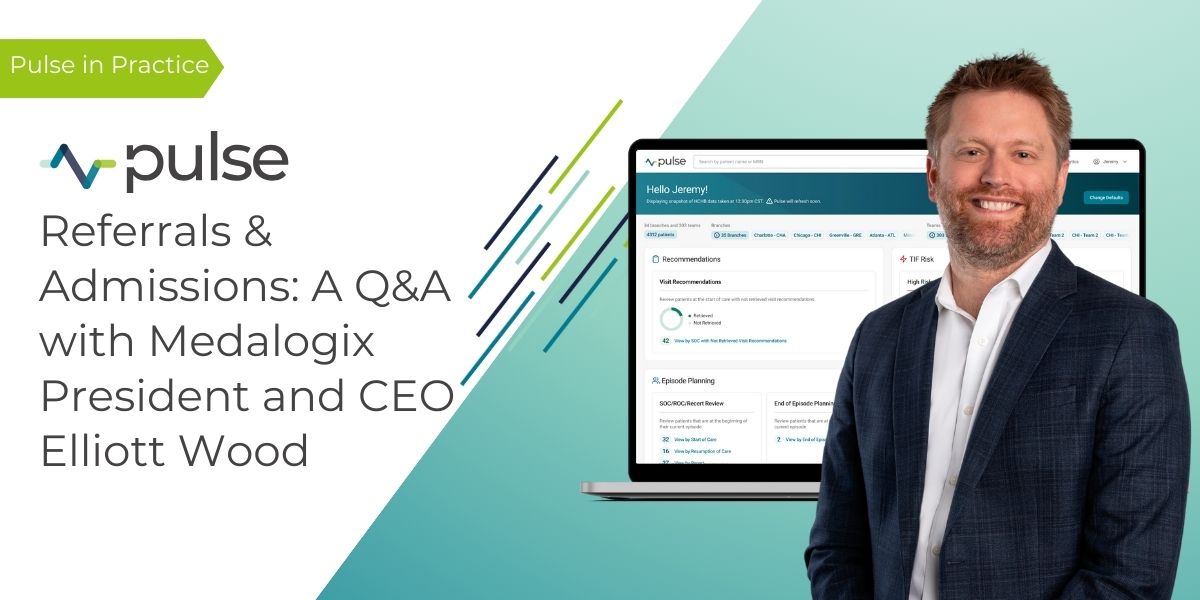
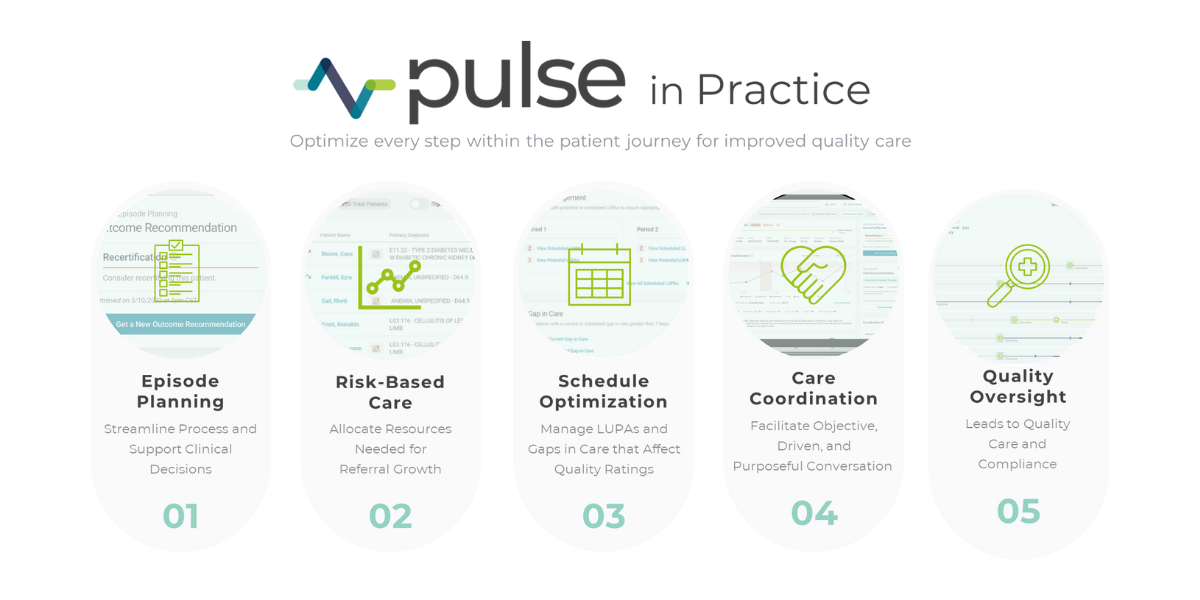
Pulse Referrals & Admissions: A Q&A with Medalogix President and CEO Elliott Wood
With our new Referrals & Admissions module now available for purchas...

MHA, Hospice Dynamix, and Medalogix Announce Partnership
SHOREVIEW, MN, February 20, 2024 — Maxwell Healthcare Associates (MHA), ...
Amedisys Finds Answer Key in Medalogix Pulse
Amedisys Expands Home Health Clinical Episode Management Partnership wit...

Transforming End-of-Life Care with Medalogix Muse at St. Croix Hospice
St. Croix Hospice, a nationally acclaimed hospice agency, has leveraged ...

The Empty Chair at the Head of the Table
Years ago, in a small, cozy house nestled in a quiet neighborhood, the f...
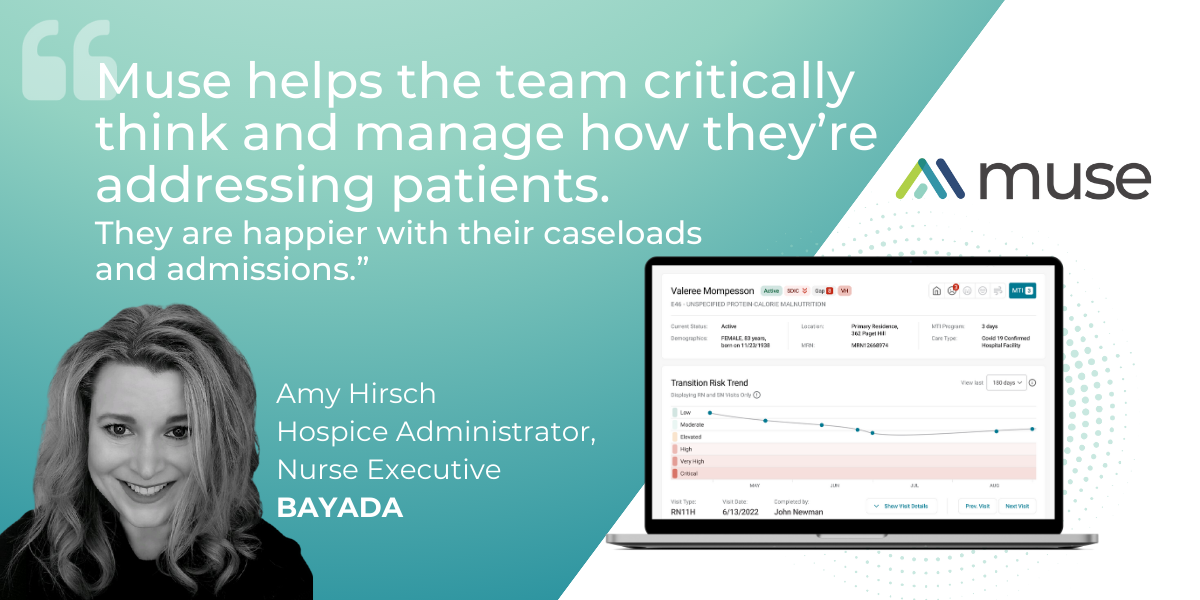
Transforming Hospice Care: The Impact of Medalogix Muse at BAYADA
In a recent interview with Amy Hirsch, Chief Clinical Officer, and Sandr...
2024 Proposed Rule: Heed the Warnings or Wait, and See?
Best Practices to Offset Impacts of 2024 Proposed Rule Providers,...
Unlocking Quality Care in Hospice: A Conversation with Medalogix and Avow Hospice
In a recent panel discussion, Medalogix's VP of Client Success and Imple...